FAQ

We understand root canal treatment may generate questions and concerns. We have attempted to answer patients’ most frequently asked questions. Please do not hesitate to contact us should you have additional questions.
What is an Endodontist?
Endodontists are dentists with at least an additional two years beyond dental school of advanced specialty training in diagnosis and treatment of root canal problems. Endodontists treat root canal problems every day and for a career.
Endodontists use their specialty training and experience in treating challenging endodontic situations, such as teeth with narrow(calcified) or blocked canals or unusual root anatomy.
Endodontists will use a variety of advanced technology such as a surgical microscope, ultrasonics, electronic apex locating devices, various anti-bacterial irrigants/medicaments, special instrumentation and obturation techniques and digital imaging, to perform this specialized treatment.
What does it mean to be ‘Board Certified’?
Education
Board Certification requires successful completion of an advanced education program in endodontics accredited by the Commission on Dental Accreditation of the American Dental Association.
To become Board Certified successful completion of three examinations is required.
The Written Examination tests a broad range of fields, including anatomy, biochemistry, pathology, immunology, microbiology, pharmacology, radiology, statistics, clinical endodontics and related disciplines.
The Case History Examination requires submission of documentation of a variety of cases from the endodontist’s own practice. The cases must be diverse and complex enough to demonstrate exceptional knowledge, skills, and expertise in the full scope of the field of endodontics.
The final phase of the Board Certification process is an Oral Examination . In the Oral Examination, a team of experts question the endodontist about a variety of endodontic diagnosis and treatment situations. Through the extensive interviews, a high level of skill in problem solving, decision making, analysis, creativity and evaluation must be demonstrated.
An endodontist, who has satisfied all requirements of the Board Certification process of the ABE, is declared Board Certified by the Directors of the ABE. This individual is a Diplomate of the American Board of Endodontics. Diplomate status needs to be maintained by successful completion of rigorous continuing education and other endodontic related activities.
Why do I need a root canal?
When the nerve of a tooth becomes infected, irreversibly inflamed or there is trauma, root canal therapy can save the affected tooth. Signs of an infected tooth can be hot or cold sensitivity, tenderness to bite, swelling, pain or a bad taste in your mouth. Some people experience no symptoms and their dentist may note a change on x-rays during a routine exam.
How do you perform root canal therapy?
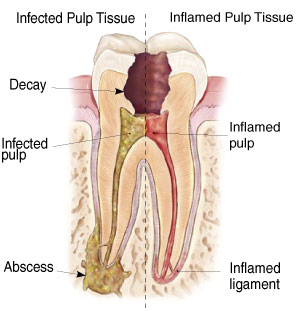
To clean the infected/affected pulp (nerve and blood vessels) the dentist will make an opening through the top of the tooth to the pulp chamber. The doctor will carefully clean out the infected/affected tissue and shape the canals to receive filling material. Images are taken to make sure that all the infected/affected pulp is removed. Typically, root canal treatment takes 1 or 2 visits. A temporary filling is placed to seal the tooth.
What are the alternatives to a root canal?
Saving your natural teeth is the very best option, if possible. Your natural teeth allow you to eat a wide variety of foods necessary to maintain proper nutrition. The root canal procedure is the treatment of choice. The only alternative to a root canal procedure is having the tooth extracted and replaced with a bridge, implant, or removable partial denture to restore chewing function and prevent adjacent teeth from shifting. These alternatives are more expensive than a root canal procedure and require more treatment time as well as additional procedures to adjacent teeth and supporting tissues. The problem with delaying treatment is that an infected tooth will never heal on its own, not even with antibiotics. This delay in treatment can lead to some very serious problems such as pain, swelling and affecting the long term retention of the tooth. As the infection spreads down the tooth and into your jawbone, the pain could become excruciating.
What is a root canal?
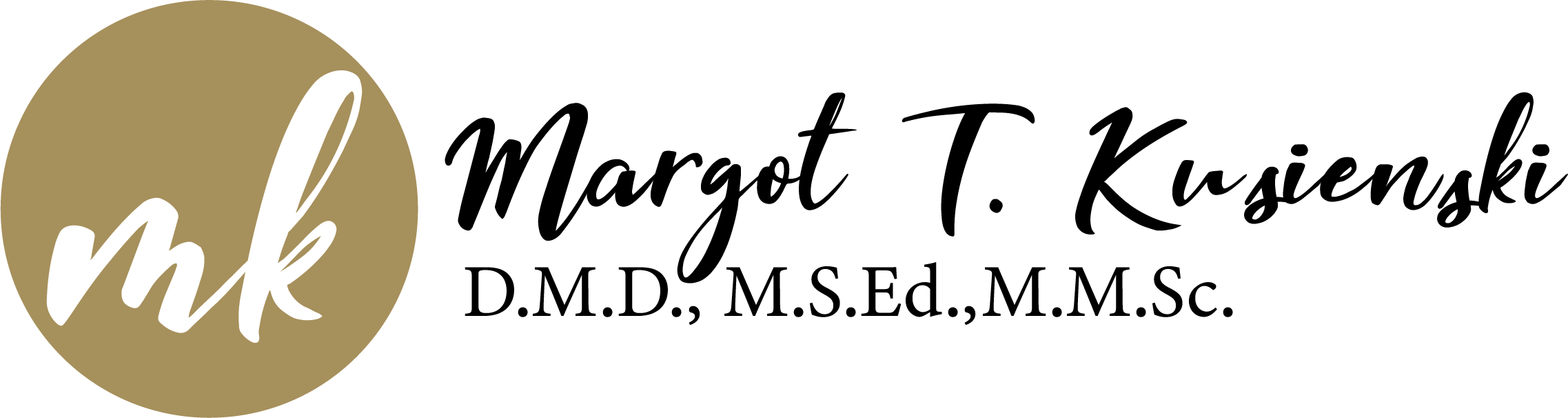
Endodontic — or root canal — treatment is necessary when the pulp, the soft tissue inside the root canal, becomes inflamed or infected. The inflammation or infection can have a variety of causes: deep decay, repeated dental procedures on the tooth, or a crack or chip in the tooth. In addition, an injury to a tooth may cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess.
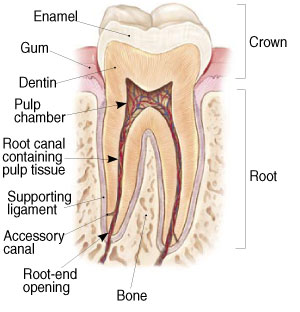
Signs to look for include pain, prolonged sensitivity to heat or cold, tenderness to touch and chewing, discoloration of the tooth, and swelling, drainage and tenderness in the lymph nodes as well as nearby bone and gingival tissues. Sometimes, however, there are no symptoms.
Root canal treatment removes the damaged pulp, or soft inner tissue containing nerves and blood vessels, from the tooth, and then the endodontist cleans, fills and seals the canals. The tooth is then restored with a permanent filling or crown (cap), allowing it to once again function normally, often for a lifetime. Root canal treatment is the only option that preserves the natural tooth.
Endodontists specialize in saving natural teeth and in performing root canals.
How much will my treatment cost?
Endodontic costs vary depending on factors such as number of roots a tooth has or type of procedure.
How long does it take?
Consultations in our office usually take 20 – 30 minutes, root canal treatment from 60 to 90 minutes.
Will it hurt?
Many endodontic procedures are performed to relieve the pain of toothaches caused by pulp inflammation or infection. With modern techniques and anesthetics, most patients report that they are comfortable during the procedure.
For the first few days after treatment, your tooth may feel sensitive, especially if there was pain or infection before the procedure. This discomfort can be relieved with over-the-counter or prescription medications. Follow our instructions carefully.
Your tooth may continue to feel slightly different from your other teeth for some time after your endodontic treatment is completed. However, if you have severe pain or pressure or pain that lasts more than a few days, call our office.
What is normal after a root canal?
Following root canal therapy, there may be some soreness in the area of the treated tooth for a few days (or even weeks) as your body begins the healing process. Areas of soreness may include the injection site, your jaw (due to being open) and where the dental dam may have been seated. These symptoms are temporary and usually respond well to over-the-counter pain medications. The amount of discomfort after the root canal is dependent on the kind and type of inflammation/infection you had when you started treatment. If swelling results after the therapy, antibiotics may be needed. If antibiotics are prescribed, it is important that you take them for the full length of time indicated on the prescription, even if the signs of infection are gone. Depending on the condition of the tooth prior to the root canal, the healing phase may be swift or slower to heal. For some people, this may take several days to a few weeks for proper resolution of the symptoms. Generally, the tooth should be back to normal within a few weeks after completion of the treatment.
Should I have feeling, pain, or sensitivity in my mouth?
Your tooth may continue to feel slightly different from your other teeth for some time after the root canal treatment has been completed. The area around the tooth can be sensitive for a few weeks after the procedure. Your tooth will be sensitive to biting pressure. This feeling is a result of the inflammation of nerve-endings in the tissue just outside the end of the root that was just treated. Discomfort in this area for a few days to a couple of weeks is common. Avoid chewing in this area until all tenderness is gone. “High” fillings are a common cause of discomfort after root canal treatment. If this occurs it will cause your tooth to stay sensitive for a longer period of time. We can adjust your bite so that your teeth don’t hurt when brought together. Anti-inflammatory medication such as Advil, Motrin, Ibuprofen are prescribed, because the body’s inflammatory reaction might lead to swelling of the tooth, making you hit it harder than the other teeth. Also, if the infection inside your tooth has spread to the bone around the root(s) end, you might be given an antibiotic after treatment; this will help with the healing process. If you continue to detect any high spots or problems with your bite, call us so we can evaluate your specific situation.
Will I be able to drive after my treatment?
You, you will. We do not use sedatives in our treatment that would affect you operating a vehicle.
How do I care for my tooth after treatment?
- Avoid chewing on the treated tooth. If possible, chew on the opposite side of your mouth.
- Continue to brush and floss normally.
- Rinse with warm salt water – dissolve a teaspoon of salt in a cup of warm water, then gently swish water around the tooth and spit, to soothe the gum, if needed.
- Take over-the-counter pain reliever, or prescribed medication as directed.
Do I need to see my dentist after the procedure?
Although the roots have permanent filling inside, the crown of the tooth has a temporary filling. If is necessary that you see your dentist within 30 days to have a permanent filling or crown put in/on the tooth. A temporary filling is placed to seal the root canal filling for a short period of time. The temporary filling does not strengthen the tooth. A permanent filling or crown must be done to insure that bacteria does not leak into the canal. Failure to do this in a timely manner can result in failure of the root canal or a possible fracture of the root resulting in the loss of the tooth. Until a permanent restoration is done, avoid chewing on the side of the treated tooth.